
Shin splints are the dreaded injury for any high school coach or athlete. Most commonly, cross country runners and track and field athletes develop this injury as a result of the high-impact nature of their sport. Potentially debilitating effects of the syndrome’s painful associated symptoms can hamper a progressive season. The need for rest becomes a priority; the periodization of training halts in place and must be completely reworked to accommodate the athlete’s rehabilitation process. Coaches should be able to recognize the key warning signs of this overuse injury, and reduce training loads accordingly, before the athlete suffers the full effect of the syndrome. Development of a smart training progression from day one and early recognition of overreaching are crucial for the athlete’s health and long-term success throughout the season and his or her career.
Biomechanics
Each foot strikes the ground approximately six hundred times every kilometer of running (Loudon & Reiman, 2012). This figure is multiplied by an impact of four to five times the athlete’s body weight transmitting sequentially, joint to joint, with each step. This impact is absorbed by every fiber in the musculoskeletal system, in succession, beginning with the point of contact in the foot, and reverberating all the way up the limbs and spine to the skull. If the runner possesses faulty biomechanics and stride efficiency, then the ground reactive forces directed irregularly up through the kinetic chain will place undue stress on specific joints, muscles, tendons, and fascia. This stress, if repetitive over time, will result in an overuse injury such as shin splints. Repetition is unavoidable in track and field athletes since the proper techniques require unidirectional propulsion, with considerable power generating from ground reactive forces through the lower body. The key is this: maximize stride economy and proper mechanics which aligns the athlete in the best possible position to absorb impact and return elastic energy all while generating the least amount of energy cost and bodily damage. More biomechanics will be introduced as we break down the injury and causation underlying the problem.
The Injury
Overuse injuries are defined by a repetitive application of submaximal stress to otherwise healthy tissues, in a manner that overwhelms the body’s natural repair process (Sando & McCambridge, 2013). Shin splints fall into the category of overuse injuries by virtue of these properties. Medial tibial stress syndrome (MTSS) is the clinical term for the colloquial slang, and it provides a description of where the primary symptoms present in the athlete. MTSS is characterized by pain in the middle to distal third of the tibia, on the posteromedial aspect of the bone (Reshef & Guelich, 2012). The area of diffuse pain measures greater than or equal to five centimeters (Sando & McCambridge, 2013). There will be pain upon palpation of that area, and mild swelling is common (Reshef & Guelich, 2012). Symptoms are present early during a workout, usually subside as exercise continues, but also can persist in some cases. Upon completion of the workout, the searing pain will return to the athlete’s shins, often exacerbated from the stress of impact. This pain should be distinguished from that of a stress fracture, which produces a focal pain, present at night, at rest, and while walking too (Sando & McCambridge, 2013).
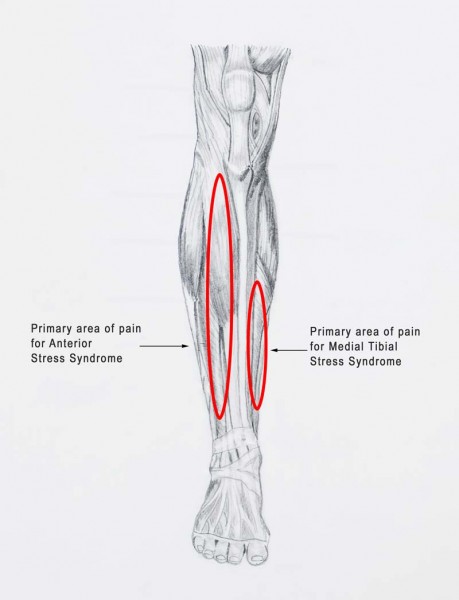
Figure 1: The regions in red show the common stress syndromes related to shin splints.
As a function of natural stride mechanics, the foot rolls from slight supination to slight pronation in a neutral runner. This motion ends with propulsion off of [primarily] the first and second metatarsal to continue the forward running motion. The soleus muscle is the prime mover of this propulsive phase of running. Individual soleus muscle fibers originate as attachments to the tibia and fibula in the lower leg, predominantly on the anterior fascia, and insert on the large calcaneal (heel) bone, blending continuously with the Achilles tendon. The soleus is made of primarily slow-twitch fibers and works most efficiently with a slightly flexed knee. The medial aspect of the soleus muscle contracts eccentrically at the moment of transition from amortization to push-off. This creates stress at the adhesion site where the soleus attaches to the fascia (Yuksel et al., 2011). Long term stress in this area leads to MTSS.
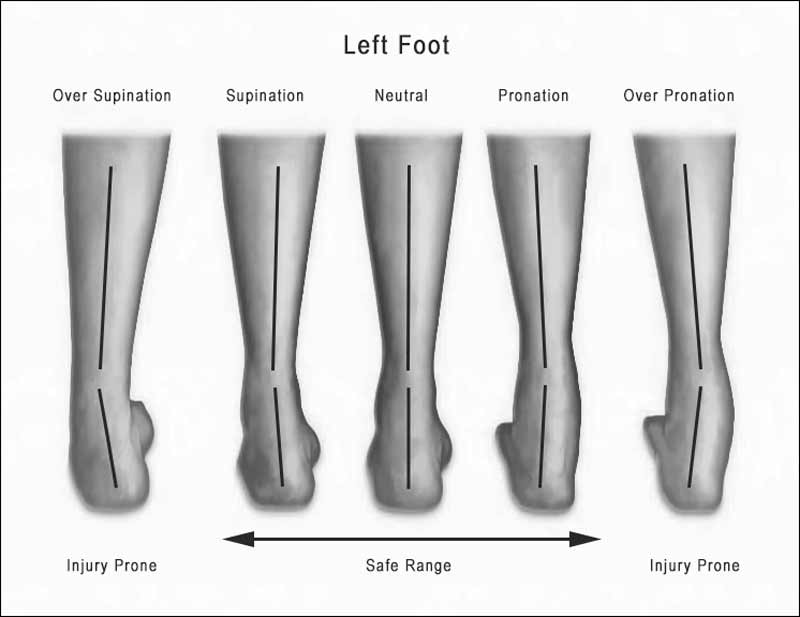
Figure 2: The overlay of lines show the angles of over supination to neutral to over pronation.
The Causes
The causes of MTSS can be categorized into two main factor groups: extrinsic and intrinsic. Extrinsic factors include the athlete’s running surface, shoes, volume and intensity of the training plan, etc. More dense running surfaces have a greater impact on the joints and require more force absorption. Worn-out shoes can place unwarranted stress on the lower limbs and often allow for overpronation and/or fallen arches. The classic model for overtraining is “too much, too fast, too soon” which brings about the need for coaches who can safely progress athletes through a season without the early demand for performance outcomes.
Intrinsic factors are both genetically and environmentally influenced. Postural anatomy is sometimes inborn, but in many cases can be adjusted and/or corrected through training. Alignment, flexibility, and strength of the ankle joint are three modifiable factors that can drastically alter biomechanical efficiency in an athlete of any age or ability (Reshef & Guelich, 2012). Muscle imbalances in any part of the system and prior injuries must also be taken into account as potential risk factors (Sando & McCambridge, 2013).
Any deviation from proper running mechanics increases the amortization phase of the ankle, and consequently, the stress on the entire system. For example, if the foot is overpronated at push-off, force is applied to an unstable structure through a closed kinetic chain; this immediately results in dissipation of elastic energy and the joints must rely on ligaments and stabilization muscles for support (Neely, 1998). The most common cause of overpronation is an imbalance of strength between invertors and evertors of the foot, in which the evertors dominate (Yuksel et al., 2011). Overpronation directly overloads the soleus and places stress on its attachment site on the medial tibia.
Loudon & Reiman (2012) investigated the deficits in pelvic, hip, or knee motion as a contributing factor to medial shin pain. The study found that greater pelvic drop and hip internal rotation as well as decreased knee flexion in a runners gait place greater stress on the lower leg; the flow chart below outlines this concept (Loudon & Reiman, 2012).
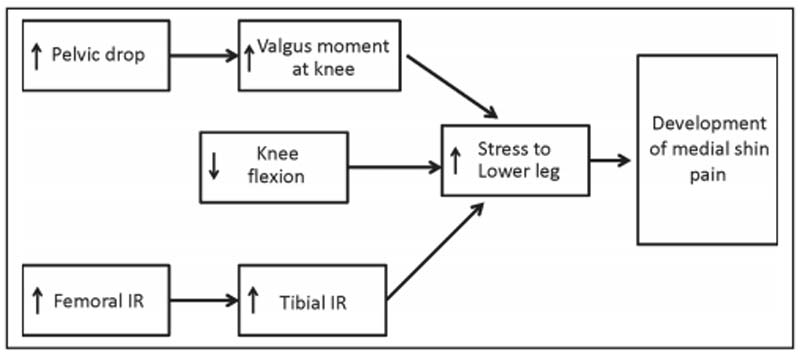
Figure 3: Conceptual model for hip contributions to distal lower extremity pathology.
Increases in pelvic tilt in the frontal plane creates a valgus knee alignment causing the medial foot to compensate with subtalar joint pronation; consider the repositioned bony attachment sites and how this applies stress on the connected muscles and tendons (Loudon & Reiman, 2012). With a decrease in knee flexion, shock dissipation is directed to the tibia and/or soft tissue rather than up through the kinetic chain (Loudon & Reiman, 2012). Some studies report that medial arch deformation, commonly known as “fallen arches,” correlates to MTSS, since it structurally simulates overpronation (Reshef & Guelich, 2012). This is also why runners with flat feet are more prone to overuse injuries such as MTSS.
The bottom line: Compensation for faulty mechanics affects the entire kinematic chain so that loss of range of motion in one joint is adjusted for in a neighboring joint, and this adjustment is always accompanied by a sacrifice in economy (Loudon & Reiman, 2012).
The Risk Factors
Female athletes are notoriously susceptible to more exercise-induced health consequences in relation to their male counterparts, simply by virtue of their genetic anatomy and physiology; these consequences include overuse injuries such as MTSS and stress fractures. Increasing average weekly mileage in high school athletes is directly proportional to male overuse injuries and female stress fractures according to one study (Tenforde, Sayres, McCurdy, Collade, Sainani, & Fredericson, 2011). Other risk factors include: body weight, body mass index (BMI), and limited range of motion in the hip (Yagi, Muneta, & Sekiya, 2013). Higher BMI and body weight places significant stress on the joints, exacerbating any malalignments and compensatory patterns. Athletes suffering from MTSS often fall into the upper range of these two categories (Yagi et al., 2013). Reshef and Guelich (2012) found cross-country runners with a BMI greater than 20 to be at a significantly greater risk of developing MTSS.
The Consequences
Athletes who continue to train through shin splints are extremely vulnerable to developing a stress fracture in one or more areas of the lower limb. A stress fracture occurs when the body is unable to absorb the shock of impact on some surface, typically due to overuse and fatiguing muscles.
Extra precaution should be taken with female runners. Both iron-deficiency anemia and amenorrhea (lack of menstruation) in women have been linked to secondary decreased bone mineral density and thus stress fractures (Yanovich, Merkel, Israeli, Evans, Erlich, & Moran, 2011). IL-6 is an inflammatory mediator in the body that responds to intensive exercise stress (Yanovich et al., 2011). When IL-6 upregulates, it induces osteoclast activity, or the breakdown of bone minerals with the intent to rebuild. However, IL-6 also activates hepcidin, a small molecule that promotes iron deficiency (Yanovich et al., 2011). Iron-deficient bone cannot rebuild itself properly, leaving the athlete in a state of weakened bone mineral density and vulnerable to stress fractures if the deficiency is not overcome. Animal studies have also shown that iron deficiency impairs the bone resorption (rebuilding) process and the root of the issue may be nothing more than an insufficiently iron-supplemented diet (Yanovich et al., 2011). Other studies have found a correlation between menstrual irregularities and the incidence of stress fractures in female athletes (Yanovich et al., 2011). A large majority of stress fractures occur in the lower leg and take a minimum of six to eight weeks to heal, creating a major setback in a competitive athlete’s training regimen regardless of the sport.
For the Coach
It is the coach’s responsibility to adjust and take care in the rehabilitation process. Weekly mileage should never capitalize by more than 10% from week to week and specifically the long run should not comprise more than 30% of the athlete’s weekly mileage. Rest is the most important factor in healing the injury in a time efficient manner. Non-impact activity such as swimming can be introduced when the athlete’s pain subsides followed by low-impact stationary biking or elliptical after a minimum of 7-10 days have passed. Depending on the severity, the athlete may need one week of complete rest before attempting any degree of activity. Soleus stretching and soft tissue massage are two therapeutic modalities that can be easily introduced after the initial inflammatory state has diminished.
Strong foundations during base-building need to be established before undergoing a heavy training load in order to avoid this potentially debilitating disorder. When an athlete is suffering from MTSS, training volume and intensity may need to be modified to give the athlete’s body a chance to recuperate and strengthen naturally. Training shoes should be replaced every 300 to 500 miles, sooner for heavier runners and those who train at high intensity. It is advantageous for runners to alternate between multiple pairs of shoes to increase the longevity of each; this also ensures that the small muscles in the feet do not adapt to identical stresses each and every day. Overpronation can be corrected with the purchase of motion control shoes and/or insoles.
Biomechanical imbalances should be addressed early in the season, or preferably the offseason, and especially when the injury red flag is thrown. Strength training emphasis should be placed on developing the invertors of the foot and eccentric strength of the soleus muscle (Tenforde et al., 2011). The foot and ankle muscles and tendons should be trained with plyometrics for maximizing spring and flexibility. Hip range of motion can be incorporated into a season-long flexibility circuit, which is performed once or twice a week; this is most easily achieved with a hurdle mobility strength series. Changing the running surface is an easy alternative for lessening the impact of a traditional workout. Track athletes should run on grass, turf, or trail as much as possible to strengthen stabilizer muscles surrounding the joints in the lower limb; this also rests the larger muscle groups subject to the pounding of the track, day in and day out.
Longevity is key for an athlete’s long-term career success. A smart coach will sacrifice short-term success for long-term progression. Psychologically, an injury setback can wreak havoc on the motivation and self-confidence of the athlete; mental strength training and positive reinforcement should not be neglected on the coach’s end. Larger dividends will pay in the long run if the proper care is taken for the athlete’s health and well-being early on. Injury prevention strategies should always take priority in a well-developed training plan, and this is ever more important in a young athlete’s growth and development.
Please share this article so others may benefit.
[mashshare]References
Loudon, J. K. & Reiman, M. P. (2012). Lower extremity kinematics in running athletes with and without a history of medial shin pain. International Journal of Sports Physical Therapy, 7(4), 356-364.
Neely, F. G. (1998). Biomechanical risk factors for exercise-related lower limb injuries. Sports Medicine, 26(6), 395-413.
Reshef, N. & Guelich, D. R. (2012). Medial tibial stress syndrome. Clinical Sports Medicine, 31, 273-290.
Sando, J. P. & McCambridge, T. M. (2013). Nontraumatic sports injuries to the lower extremities. Sports Medicine Update: clinical Pediatric Emergency Medicine, 14(4), 332-339.
Tenforde, A. S., Sayres, L. C., McCurdy, M. L., Collade, H., Sainani, K. L. & Fredericson, M. (2011). Overuse injuries in high school runners: Lifetime prevalence and prevention strategies. Physical Medicine and Rehabilitation, 3, 125-131.
Yagi, S., Muneta, T., & Sekiya, I. (2013). Incidence and risk factors for medial tibial stress syndrome and tibial stress fracture in high school runners. Knee Surgery, Sports Traumatology, Arthroscopy, 21, 556-563.
Yanovich, R., Merkel, D., Israeli, E., Evans, R.K., Erlich, T., and Moran, D.S. (2011). Anemia, iron deficiency, and stress fractures in female combatants during 16 months. Journal of Strength & Conditioning Research, 25(12), 3412–3421.
Yuksel, O., Ozgurbuz, C., Ergun, M., Isleen, C., Taskiran, E., Denerel, N., & Ertat, A. (2011). Inversion/eversion strength dysbalance in patients with medial tibial stress syndrome. Journal of Sports Science and Medicine, 10, 737-742.

Shin splints are usually caused by repeated trauma to the connective muscle tissue surrounding the tibia.
They are a common injury affecting athletes who engage in running sports or other forms of physical activity, including running and jumping.
They are characterized by general pain in the lower region of the leg between the knee and the ankle.
Shin splints injuries are specifically located in the middle to lower thirds of the inside or medial side of the tibia, which is the larger of two bones comprising the lower leg.